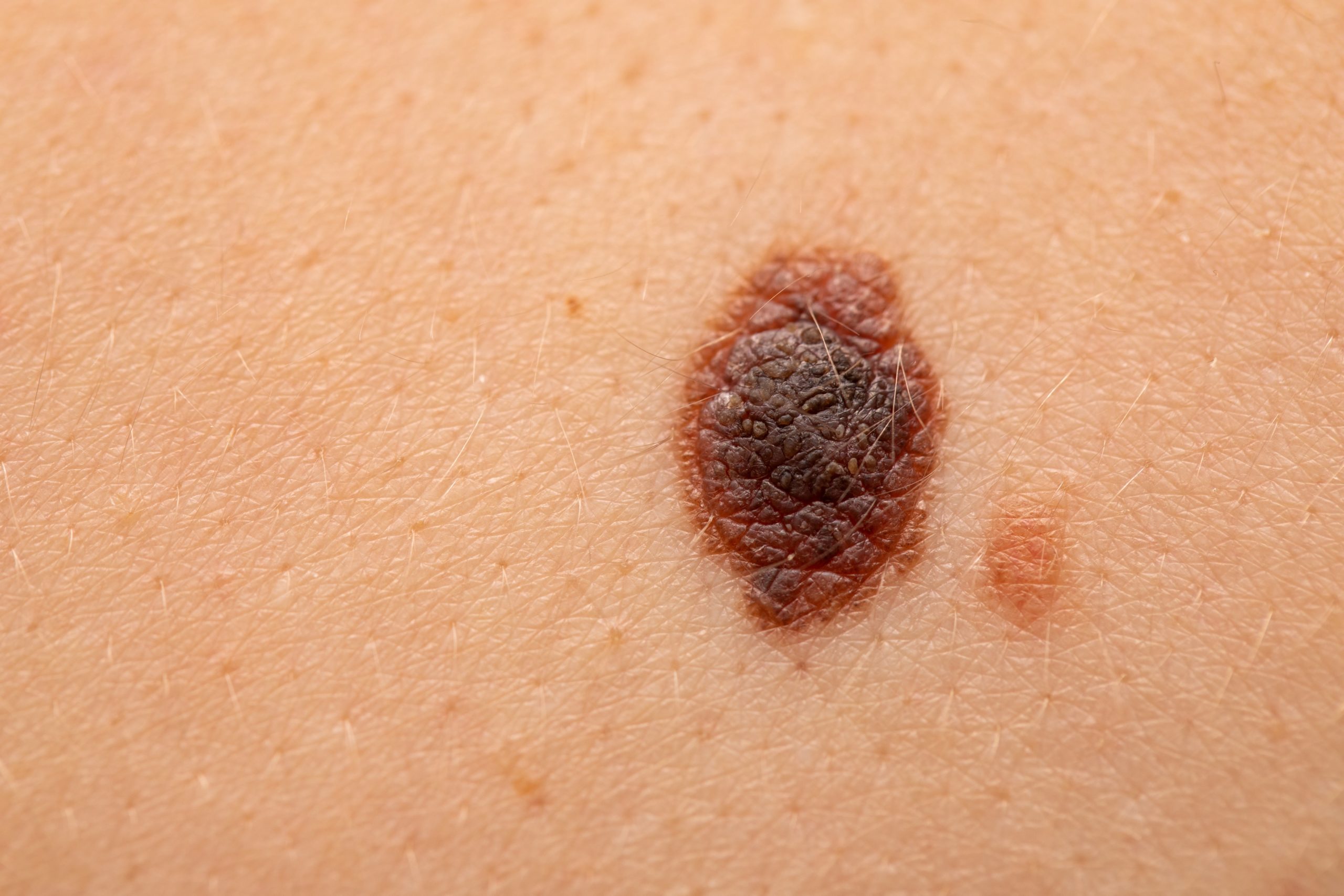
Malignant melanoma today: where are we now and where will we go? Pt.3
| 19 May 2022
0 Replies
DESCRIPTION
ABSTRACT
In this section, the focus is on the role of PDL-1 both as a diagnostic and predictive biomarker in malignant melanoma.
Text.
Another important aspect of the histopathological diagnosis of malignant melanoma is related to the use of immunohistochemical markers, both as a diagnostic aid (discussed extensively in the previous sections) and as a predictive marker of response to various drugs.
For example, very recently, the use of Pembrolizumab (immune checkpoint inhibitor) in the treatment of metastatic or unresectable melanoma was approved by AIFA.
In this scenario, an extremely important role is played by immunostaining for PDL-1 performed with various and different platforms, on tissue previously removed from the patient in question. To do this, the various centers have equipped themselves to conduct an adequate immunohistochemical analysis, similarly to what has already been happening for some years for other neoplasms, including non-small cell lung cancer (NSCLC).
According to this perspective, the sections with a thickness of about 5 microns are subjected to staining with adequate antibodies, without glue, and the results are observed under an optical microscope, similarly to any other immunoreactions with antibodies of the most varied.
By doing so, a semi-quantitative evaluation of the chromogenic signal is prepared, considering only the neoplastic tissue (and therefore, without the presence of inflammatory elements as, for example, occurs in the case of head / neck neoplasms), and the cut-off is positioned at three different levels of significance:
- Negative for immunoexpression: 0% (therefore, no melanoma cells express membrane immunolabeling for PDL-1);
- Low expression of PDL-1: 1-49%, fairly large cut-off that allows to classify in this way, different types of positivity for this marker;
- High PDL-1 expression: > 50%, i.e. more than half of the representative cells of the study sample, are immunostained with anti-PDL-1 antibody.
In doing so, depending on the results of the immunohistochemical observation, the medical oncologist will be able to make a precise decision on which line of therapy to administer to the patient, allowing or not, depending on the reading result, to be able to administer a given immune checkpoint inhibitor.
From what has been said and explained above, it is clear that the pathologist's role does not end only in providing a given diagnosis, an indispensable basis on which to build the patient's entire diagnostic-therapeutic pathway, but also it is an indispensable task of the dermatopathologist to provide the clinician fundamental parameters, such as to modify and / or orient future therapeutic choices.
Lascia un commento