Malignant melanoma today: where are we now and where will we go? Pt.1 (general part)
| 10 March 2022
0 Replies
DESCRIPTION
ABSTRACT
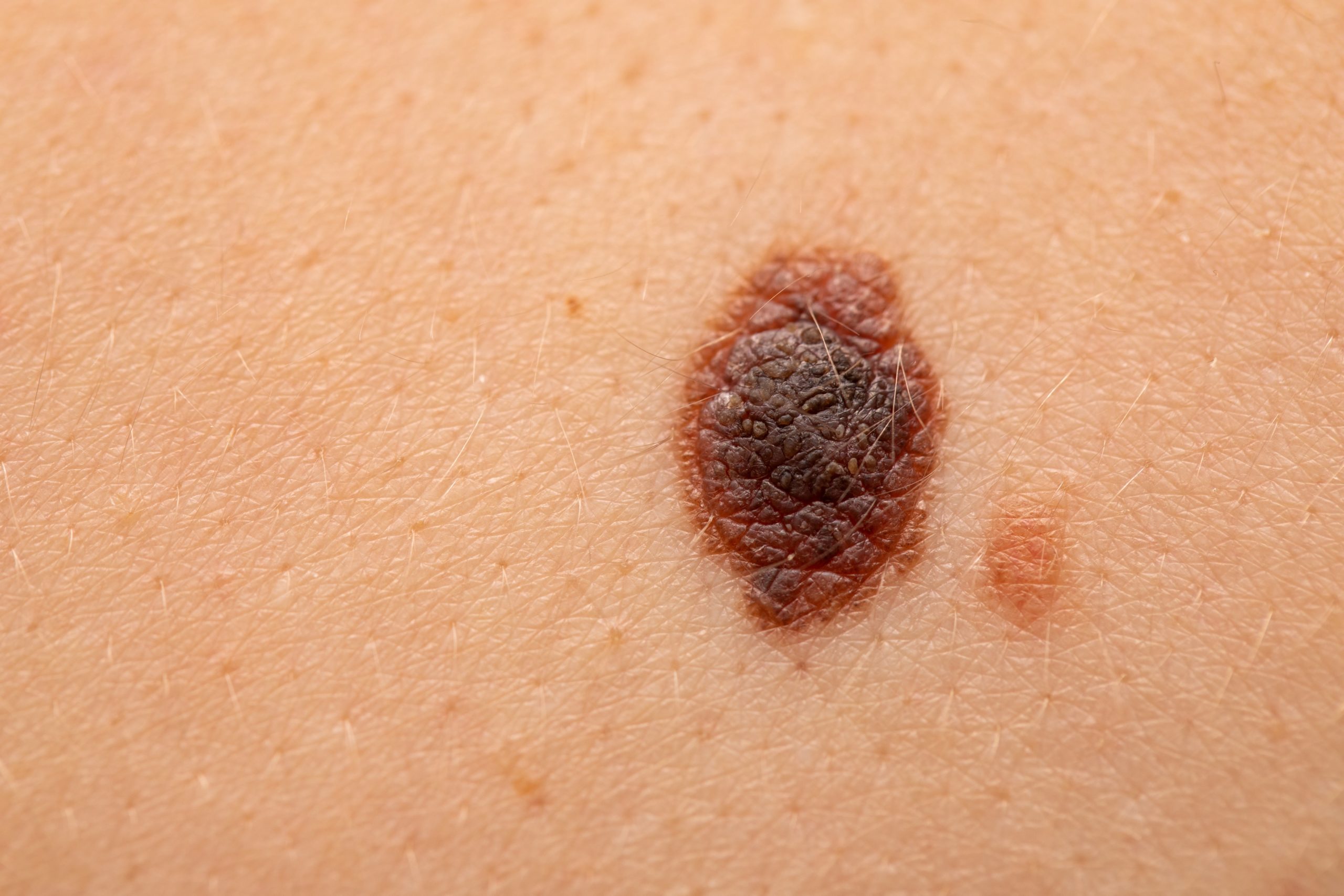
Malignant melanoma (MM) represents the most aggressive skin cancer and, despite advances in therapy and treatment. There are about 324,635 new cases and 57,043 Deaths worldwide in 2020, accounting for 1.7% of all cancers in the world population and showing a rising incidence. Since the arbores of dermatopathology, MM has been a challenge, both in terms of diagnosis and nosographic categorization. In fact, for a long time they were called "melanoma" morphologically atypical lesions, which, however, did not show aggressive behaviour and, conversely, morphologically not completely dysplastic lesions, which instead showed a completely invasive biology. In the course of this journey we will explore this reality closely, face the difficulties we face on a daily basis and eventually introduce the use of algorithm-based artificial intelligence as a potential aid in dermatopathological diagnostics.
Malignant melanoma (MM) represents the most aggressive skin cancer and, despite advances in therapy and treatment. There are about 324,635 new cases and 57,043 Deaths worldwide in 2020, accounting for 1.7% of all cancers in the world population and showing a rising incidence.
Since the arbors of dermatopathology, MM has been a challenge, both in terms of diagnosis and nosographic categorization. In fact, for a long time they were called "melanoma" morphologically atypical lesions, which, however, did not show aggressive behavior and, conversely, morphologically not completely dysplastic lesions, which instead showed a completely invasive biology.
This led to the discovery, for example, of how reported cases of "juvenile melanoma" by Sophie Spitz were melanocytic lesions with non-aggressive behavior, and, therefore, not to be categorized tout-court as MM.
Over the years the advent of immunohistochemistry as an ancellary technique has allowed to increase the sensitivity, specificity and therefore diagnostic accuracy in the recognition of melanocytic lesions, allowing a faster and safer identification. There is no doubt, however, that not all diagnostic difficulties have been overcome, as histotypes of MM exist that are difficult to diagnose without adequate experience and years of preparation. We think of Melanoma Desmoplastic, an uncommon variant of MM that loses the classic markers of melanocytic differentiation known as Melan-A (MART1) and HMB-45 (Melanoma-Ag) e, whose diagnostic suspicion is essential to require additional markers represented mainly by SOX-10, in addition to MITF and Tyrosinase.
On the other hand, it is important to underline how the diagnostic difficulties are "double-track", as even making a diagnosis of benign injury requires a certain rigour and experience. In a very famous and widespread book in the community of dermatopathologists there is a reference to a kind of flash phrase, which all of us should keep in mind: the authors wonder what could be the worst mistake for an anatomist-pathologist? Not recognizing malignant melanoma as benign lesions. Here, also today, at the beginning of 2022, the histological diagnosis of MM continues to represent the gold standard, even in the presence of fast and rapid evolution of the new molecular biology techniques that we will deepen along this journey.
In addition to all these aspects, we must reflect on the origin of the cells from which MM comes. Melanocytes, in fact, are cells of neuroectodermal derivation, that is, both, during the embryonic development, are cytotypes that migrate from the "crista neuralis" up to localize in the skin, but during their journey they "move" in the true sense of the term. This embryological reminiscence is of fundamental importance to explain why it is possible to describe particular forms of melanoma in places where there is apparently no expectation (primary melanoma of the gastrointestinal tract) but it is also of fundamental importance for the pathologist when, during the evaluation of the sentinel lymph node excisions for MM, we are faced with intra or subcapsular snowy inclusions, which must be appropriately differentiated by a metastasis (micro or macrometastasis) of MM. Sometimes this can create real headaches of differential diagnosis.
In the course of this journey we will explore this reality closely, face the difficulties we face on a daily basis and eventually introduce the use of algorithm-based artificial intelligence as a potential aid in dermatopathological diagnostics.
To be continued...
Lascia un commento