
Malignant melanoma today: where are we now and where will we go? Pt.2 (requirements)
| 12 April 2022
0 Replies
DESCRIPTION
ABSTRACT
Malignant melanoma (MM) represents the most aggressive skin cancer and, despite advances in therapy and treatment. There are about 324,635 new cases and 57,043 Deaths worldwide in 2020, accounting for 1.7% of all cancers in the world population and showing a rising incidence.
Since the arbores of dermatopathology, MM has been a challenge, both in terms of diagnosis and nosographic categorization. In fact, for a long time they were called "melanoma" morphologically atypical lesions, which, however, did not show aggressive behaviour and, conversely, morphologically not completely dysplastic lesions, which instead showed a completely invasive biology.
In the course of this journey we will explore this reality closely, face the difficulties we face on a daily basis and eventually introduce the use of algorithm-based artificial intelligence as a potential aid in dermatopathological diagnostics.
As we began to discuss last time, histopathological diagnosis of malignant melanoma continues to be the gold standard in the diagnostic-therapeutic care (PDTA) of the patient with Malignant Melanoma (MM).
Although, in fact, in the last two decades and more particularly in recent years there has been an unprecedented development of the techniques of molecular biology (Next Generation Sequencing, NGS, for example), the morphology is completely imprenscindibile for the correct nosographic framing of a cutaneous lesion suspected of constituting a melanoma.
In calculating the different types of information, a good histopathological report cannot ignore information that is essential, easily accessible and (at least in the intentions!) reproducible.
There are various histotypes of MM whose recognition is fundamental to report this entity correctly on the histopathological report. Depending on the arrangement of melanocyte cells we distinguish the Superficial Spreading Type Melanoma (SSM), the Lentigo-maligna type Melanoma, the pagetoid-pattern melanoma, the nested-pattern melanoma, the nevoide melanoma, desmoplastic/spindle cells melanoma and other less common histological types.
From the strictly prognostic point of view the difference between the different histotypes is important to understand the melanomas that develop on the skin with scleroelastosic damage compared to the melanomas that develop on the skin without or with low scleroelastosic damage (WHO 2018, CSD: Cumulative Solar Damage) [1].
Another very important parameter to be evaluated, the most significant in absolute, is the thickness according to Breslow, that is the measurement of the point of maximum infiltration of melanomatous cells starting from the grainy state of the epidermis.
The guidelines and daily practice suggest that the use of a computer measurement device is able to ensure excellent measurement accuracy as well as greater reproducibility of the data. Do not forget, in fact, that the thickness of Breslow governs the prognosis of the subject with MM: the greater the thickness of the lesion, the greater and more aggressive will be the treatments to which the subject will be subjected in an attempt to reduce the risk of disease progression.
In figure 1 we can see an example of the concept of thickness of Breslow applied to melanomas of the head/neck district. The concept remains the same: as vertical development increases, the risk of worse outcomes increases, and therefore more surgery/oncology is needed.
In Figure 2 we observe the last edition, currently used (AJCC 8'Edition), relative to the post-pathological staging (pTNM) of the MM: we follow cut-offs related to values ranging from stage pT1a to stage pT4b. Survival rates, overall survival rates, free-survival progression rates, and other values are reduced rather proportionally as the pTNM stage progresses. Another parameter considered important but now almost not used is represented by the level of Clark: it is a measurement on a topographical basis of the area of skin, dermis and possibly subcutaneous infiltrated by MM.
In figure 3 we can appreciate an example of measurement of the level according to Clark: depending on whether the tumor infiltrates the superficial dermis (papillary), the reticular dermis (deep), or the subcutaneous will be assigned a level of Clark.
We said, however, that this parameter has fallen into disuse, because the absence of objective criteria of measurement has made difficult the inter-observer reproducibility.
A third important element is represented by ulceration: this term refers to any continuous solution of the epidermis linked to the spread of melanoma. As can be easily understood from the figures cited, in particular Figure 2, the presence or absence of ulceration plays a fundamental role in the passage of a lesion with the same thickness (for example 0.6 mm) in a category such as pT1a or pT1b.
In fact, it is enough that the lesion is ulcerated to upgrade the stage to a higher level. In recent times, an increasing interest in this parameter has led to the conduct of studies to assess whether the radial extension of ulceration could have an impact on the prognosis of patients. To be continued…
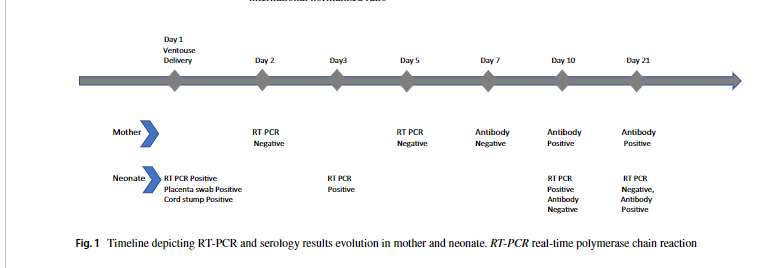
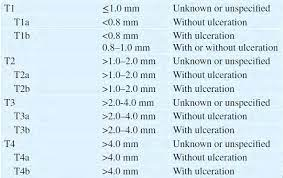
Figure 2. Summary image of the pTNM system (p: pathological, T: tumor, N: node, M: metastasis) currently used (AJCC 8'Edition).
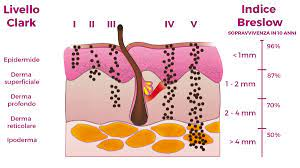
Figure 3. Example of how the level is measured according to Clark.
References
- WHO Classification of Skin Tumours, WHO Classification of Tumours, 4th Edition, Volume 11.
Lascia un commento