
SARS-CoV-2 and Placenta: A new but very tangled story
| 24 February 2022
0 Replies
DESCRIPTION
Premise and presentation of the cycle “SARS-CoV-2 and Placenta”
Since the first pandemic months, many and different aspects related to the SARS-CoV-2 infection have been brought to light, with evident difficulties in relation to the recovery of cases that could be educational and harbingers of new scientific knowledge. This premise, although valid in every different context, has proved particularly valid for the discourse relating to expectant mothers who were infected with the disease. Therefore, in the first semester of the pandemic, even an accurate search in the literature would have produced few results on the issue of Covid-19 in pregnant women and, even more, on the potential risk of maternal-fetal (vertical) transmission linked to the virus.
Having said this, in the coming months we will venture into this topic by following the most significant stages of the discoveries, we will focus in particular on what are the actual "footprints" that SARS-CoV-2 is able to "leave" at the level of the placental parenchyma, and we will try to trace future challenges and perspectives, in consideration of the advent of new variants (Omicron in primis), on the possible involvement of newborns.
One of the earliest contributions in the literature came from the article by Hosier et al.,published in early 2020 in the Journal of Clinical Investigations (JCI) in which the authors described a single case of an American, an Asian, non-Asian patient. Hispanic, aged 35, with no significant medical history except for psoriasis not in clinical disease activity. The patient had been infected by her husband who had had direct contact with a SARS-CoV-2 positive subject. The woman was in the second trimester of pregnancy, and, after careful medical history, had reported a previous pregnancy in which a condition of elevated blood pressure had occurred, suggesting pre-eclampsia. At the time of the ascertained positivity to the virus, the woman had rather good vital signs except the triad of signs represented by: elevated blood pressure (150/100 mmHg), thrombocytopenia and elevation of liver enzymes (transaminases). These 3 conditions were sufficient to suspect that a form of severe pre-eclampsia was about to occur. In the following days, in order not to risk increasing maternal morbidity or death, termination of pregnancy (IVG) was chosen and biological samples were recovered for a detailed analysis of pathological anatomy.
Optical microscopy highlighted an excess deposit of intervillous and perivillous fibrin, with the presence of inflammatory lymphocyte cells (CD3 +) and the monocyte-macrophage system (CD68 +) (Figure 1). In addition, immunoreactions were performed for anti-SARS-Cov-2 S1 glycoprotein which showed the presence of a signal on the syncytiotrophoblast cells, i.e. the external part of multinucleated cells that act as an interface between maternal and fetal blood, allowing not only exchanges of metabolites (nutrients and waste products) but also of being able to carry any infectious agents (such as Cytomegalovirus, Toxoplasma Gondii, etc). A further investigation by means of the electron microscope made it possible to find particles of the order of nanometers (nm) that could be interpreted as SARS-CoV-2 virions (we will focus on the correct interpretation of the ME images in the cycle of the next meetings) (Figure 2).
On the basis of all this information, it was deduced that, with reasonable certainty, the symptomatic infection with SARS-CoV-2 had caused a worsening of the conditions (already basic) tending to gestational hypertension, and therefore to pre-eclampsia. This first case reported in the literature opened the door to a hitherto unexplored world, mechanisms of immunophysiopathology that were not yet fully understood began to be postulated and stimulated active research on these issues by researchers from all over the globe.
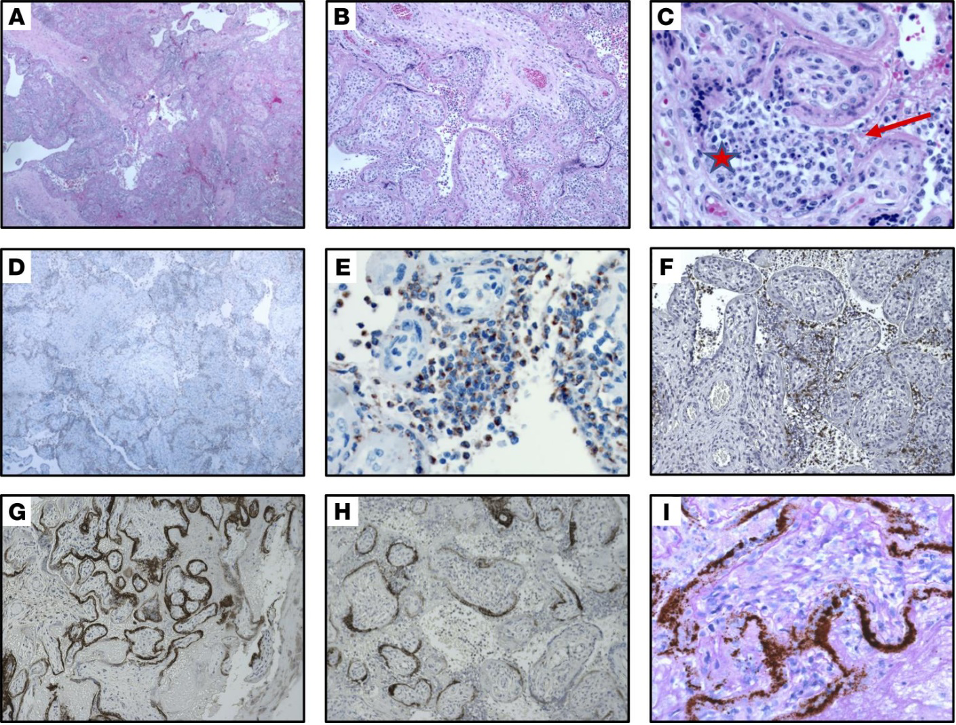
(A–C). Section of placenta stained with H&E showing histiocytic intervillositis. Original magnification, ×40 (A), ×100 (B), ×400 (C). (C) Star indicates intervillous space infiltrated by immune cells. Arrow indicates perivillous fibrin. (D and E). Immunohistochemical stain for CD68 showing the majority of intervillous inflammatory infiltrate positive (brown stain) for this macrophage marker. Original magnification, ×40 (D), ×400 (E). (F) Staining for CD3, a marker of T lymphocytes. Original magnification, ×100. (G and H). Immunohistochemical staining for SARS–CoV-2 spike protein, demonstrating virus localization predominantly in syncytiotrophoblast cells. Original magnification, ×50 (G), ×400 (H). (I) In situ analysis for the presence of SARS–CoV-2 RNA shows strong positive staining within the placenta . Original magnification, ×400. (Hosier H, Farhadian SF, Morotti RA, Deshmukh U, Lu-Culligan A, Campbell KH, Yasumoto Y, Vogels CB, Casanovas-Massana A, Vijayakumar P, Geng B, Odio CD, Fournier J, Brito AF, Fauver JR, Liu F, Alpert T, Tal R, Szigeti-Buck K, Perincheri S, Larsen C, Gariepy AM, Aguilar G, Fardelmann KL, Harigopal M, Taylor HS, Pettker CM, Wyllie AL, Cruz CD, Ring AM, Grubaugh ND, Ko AI, Horvath TL, Iwasaki A, Reddy UM, Lipkind HS. SARS-CoV-2 infection of the placenta. J Clin Invest. 2020 Sep 1;130(9):4947-4953. doi: 10.1172/JCI139569. PMID: 32573498; PMCID: PMC7456249.)
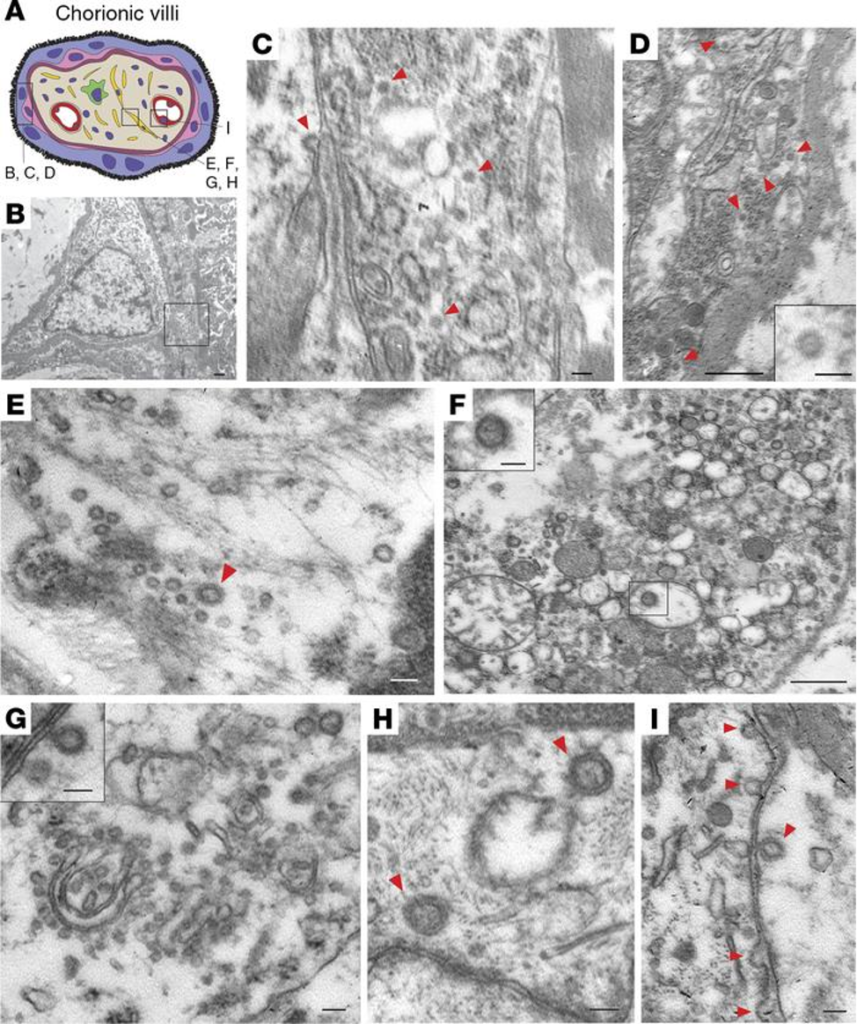
(A) Schematic illustration of chorionic villi. Cytotrophoblasts, syncytiotrophoblasts, fibroblasts, and endothelial cells are indicated in pink, purple, yellow, and red, respectively. (B) Cytotrophoblast (on the left with the nucleus) and syncytiotrophoblast (on the right). Scale bar: 500 nm. (C) Enlarged image of boxed area in B. Cytoplasm of a syncytiotrophoblast cell with virus particles (red arrowheads). Scale bar: 100 nm. (D) Cytoplasm of a cytotrophoblast cell with virus particles indicated by red arrowheads. Scale bar: 500 nm and 100 nm (insert). (E–H) Fibroblast with virus particles indicated by red arrowheads. Scale bars: 100 nm (E), 500 nm (F) (insert, 100 nm), 100 nm (G) (insert, 100 nm), 100 nm (H). (I) Endothelial cell within chorionic villus with budding viral particles indicated by red arrowheads. Scale bar: 100 nm. (Hosier H, Farhadian SF, Morotti RA, Deshmukh U, Lu-Culligan A, Campbell KH, Yasumoto Y, Vogels CB, Casanovas-Massana A, Vijayakumar P, Geng B, Odio CD, Fournier J, Brito AF, Fauver JR, Liu F, Alpert T, Tal R, Szigeti-Buck K, Perincheri S, Larsen C, Gariepy AM, Aguilar G, Fardelmann KL, Harigopal M, Taylor HS, Pettker CM, Wyllie AL, Cruz CD, Ring AM, Grubaugh ND, Ko AI, Horvath TL, Iwasaki A, Reddy UM, Lipkind HS. SARS-CoV-2 infection of the placenta. J Clin Invest. 2020 Sep 1;130(9):4947-4953. doi: 10.1172/JCI139569. PMID: 32573498; PMCID: PMC7456249.)
Lascia un commento