
SARS-CoV-2 and the newborn: what do we know? (Pt.1)
| 29 March 2022
0 Replies
DESCRIPTION
ABSTRACT
Although initially rare and anecdotal, reports of likely vertical transmissions of SARS-CoV-2 have increased in the last months of the pandemic. Today we discuss one of the first reports presented in Literature in 2021, when very little was still known about this topic.
In Literature, one of the first cases of vertical transmission to have been described, is due to Kulkarni et Al., who reported the experience of a 24-year-old girl who arrived, at 38 weeks + 2 days of gestation, presenting symptoms such as fever, loss of appetite and muscle aches.
The patient was in labor and, therefore, all procedures were in place to minimize the possibility of infection, in the event of a positive SARS-CoV-2 (N95 masks, visors, long-sleeved shirts and sterile gloves). The child was placed in a tray for childbirth with a sterile cloth and immediately transferred to resuscitation by a pediatrician.
Delayed cable locking or skin-to-skin contact was not performed. The child did not require any resuscitation at birth and was awarded APGAR scores of six and nine to one and 5 minutes of life.
No oropharyngeal or nasal aspiration was performed. The birth weight was 3200 g.
The child was transferred to a separate neonatal room with air and contact isolation precautions according to the guidelines of the Indian Council of Medical Research (ICMR). The child was fed formula and had no contact with any family member.
Reverse transcriptase (RT) PCR was performed on nasopharyngeal aspirate (NPA), umbilical cord stump, and placenta at birth.
All samples were collected under strict aseptic precautions to ensure zero contamination. The child’s NPA, umbilical cord stump and placenta were reported to be positive for SARS-CoV2 at 12 hours of life. The mother tested negative for SARS-CoV2 at the first swab (collected at admission) and again on day 5. At 38 hours of life, the child was found with fever, jaundice and poor nutrition.
A provisional clinical diagnosis of neonatal sepsis was made and EV antibiotics (ampicillin plus gentamicin) were started immediately after the collection of blood cultures and other tests for neonatal sepsis.
The cerebrospinal fluid was run which revealed five cells (all lymphocytes) with normal protein and sugar. There was no ABO or Rh incompatibility and the direct Coomb test was negative.
Over the next 2 days, the child continued to experience fever peaks, and investigations showed thrombocytopenia and elevated inflammatory markers (CRP/Procalcytonine/Ferritin) with high d-dimers (Table 1). Antibiotics were changed to Meropenem and Vancomycin and the decision was made to add Lopinavir Ritonavir (as an antiviral drug for SARS-CoV2, extrapolating evidence from use in newborns for HIV) and IVIG due to a clinically significant disease with very high inflammatory markers. Chest X-rays, EKG and 2D echo were normal. Antibiotics were suspended after negative reports on the culture.
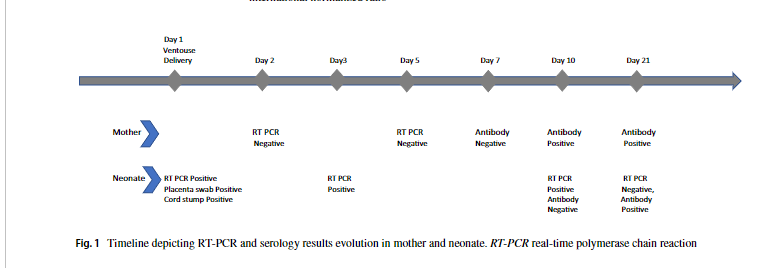
The nasopharyngeal buffer of the newborn for SARS-CoV-2 RT-PCR, obtained at childbirth, was positive. RT-PCR repeated on day 5 and day 10 was positive. Maternal serology on day 2 after childbirth was negative for antibodies, followed by antibodies positive to the test repeated on day 10 after childbirth (day 11 after the onset of symptoms in the mother, titres 10,26 COI) and 21 (titres 87,68 COI). The child tested negative for antibodies on day 10 but tested positive for antibodies on day 21 (COL titres 5.25). Figura 1.
Table 1. Clinical results of infant.
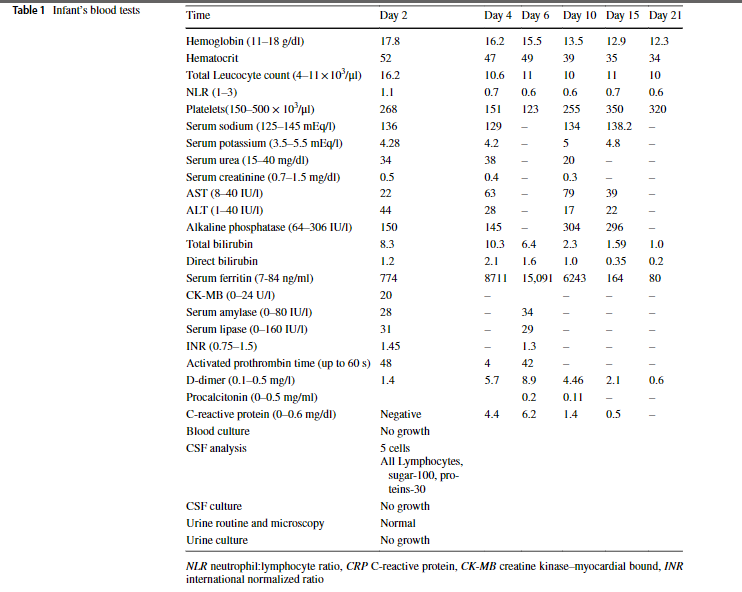
Figure 1. The time sequence describing the evolution of RT-PCR and serology results in the mother and newborn. RT-PCR: real-time polymerase chain reaction.
On the 14th, the child showed a negative SARS-CoV-2 swab and was discharged from the hospital on the 21st.
Until the publication date of this interesting case report, only 2 other cases of vertical transmission of SARS-CoV-2 had been described in the Literature. Over the next few months, new acquisitions demonstrated how placental parenchyma behaves as a "screen" in an attempt to block the transmission of virions to the fetus. In the next article we will examine a systematic review of the Literature that has made it possible to summarize the knowledge we have so far about this.
Lascia un commento